Post-Operative Instructions for Breast Augmentation
Medications After Breast Augmentation
- Pain: You will be prescribed a pain medication for post-operative pain control. If your discomfort after surgery is not strong you are welcomed to take Tylenol in place of the prescribed medication. Do not take Tylenol with the pain medication, often the medication you are prescribed will have Tylenol in it. Do not exceed 4,000 mg of Tylenol in any 24-hour period. Take medication with food to minimize risk of nausea.
- Nausea: A common side effect after general anesthesia and strong medications. If you are experiencing nausea, we advise that you take your nausea medication.
- Constipation: You will experience constipation if taking narcotic pain relievers. MiraLAX or other over the counter laxatives are recommended. Do not wait to take until you are constipated.
- Medications to Avoid: Take only those medications approved or prescribed by your surgeon.
Nutrition After Breast Augmentation
- Diet: A light low-fat diet is best after surgery. You may start a regular diet the day after surgery if you are not feeling nauseous or vomiting. Start with liquids for the first few hours after surgery and then slowly advance to more solid foods.
- Hydration: Stay hydrated by drinking 8 -10 glasses of water a day. Avoid alcohol for 48 hours and while you are still taking pain medications.
Activity After Breast Augmentation
- Movement is Important: Make sure to get out of bed and maintain movement (walking around) immediately after your surgery. When lying down in bed or on the couch, make sure you are moving your legs and ankles. Take deep breaths frequently to keep your lungs clear.
- Sleep: Sleep on your back with your head elevated about 30-40 degrees (2-3 pillows). Do not sleep on your side. Keeping your body more upright will minimize swelling. Continue this for one week.
- Exercise: Light physical activity may be resumed 2-3 weeks after surgery. Remember to start easy and build back up to your previous exercise levels. At 6-8 weeks or when further instructed by your surgeon, more intense exercise can be started. Just know that swelling may transiently be worse with exercise.
- Arm Movement: Limit your arm use to daily activities such as brushing your teeth, eating, and combing/shampooing your hair. Avoid rigorous movement and do not lift more than 5 lbs. Let pain be your limiting factor. If it hurts, please do not do it.
- Compression Bra: Expect to wear a special bra for the entire first week after surgery and then as recommended by your surgeon. The bra should fit snug but not too tight. The surgical bra is to provide support while you heal from surgery.
- Driving: DO NOT operate a vehicle or make important decisions until you have been off pain medications for 24 hours. Use good judgment.
- Return to work: Most patients require approximately 5-7 days off work depending on their job responsibilities. Returning to work with a light schedule initially or even parttime can be beneficial as well.
- Sexual Intercourse: Sexual activity can be resumed when you feel ready with no restrictions. Incisions should be well healed. Patients typically feel ready after one month.
- Displacement Exercises: Unless instructed otherwise, breast exercises are not needed after a breast augmentation. This is particularly true if anatomical-shaped implants have been used. These maneuvers can cause malrotation of the shaped devices. If it appears in your follow-up evaluations that stretching is needed along the lower portion of the breasts, these exercises may be advised. Your surgeon will provide any necessary instruction at that time.
- Sleeping: It is advised for the first few weeks to sleep on your side or your back to avoid putting too much pressure on the breasts.
- Showering: You may shower with assistance the day following surgery. Remove your bra. Incisions are covered with a waterproof dressing and require no special attention. Put your bra back on after your shower.
How To Take Care Of Your Incisions After Breast Augmentation
- Incisions: Your incisions are covered with a waterproof dressing. No dressing changes or incision care is required. After your first postop visit, the dressing will be removed, and tape will be applied. This special brown tape helps with scar healing and improves the appearance of your scar. Continue to cover your incision sites with the brown tape for as long as your surgeon suggests.
- Stitches: All stitches are dissolvable.
- Scar ointment: Scars are small and hidden in the breast crease. They may take up to a year to fully heal. After your incisions have completely healed and when your doctor has told you it is safe, you can begin to use silicon-based ointment on your scars to improve healing.
What To Expect After Breast Augmentation
- Bruising: You can expect to have bruising. Most bruising will resolve after about 2-3 weeks. The bruise will go from a purplish color to a yellow/green shade as it starts to resolve.
- Swelling: You can expect swelling particularly in the top half of the breasts. This can take 3-4 weeks to improve and the swelling is responsible for the feeling that the implants are high. As the swelling resolves, it seems as though the implants drop into a lower position.
- Itching: Itching at the incision sites is normal for a few days. You may take Benadryl to help with this.
- Pain: It is normal to experience tightness, pressure, soreness, itchiness, and fatigue for several days to weeks following surgery as your skin and muscle adjust to your breast implants.
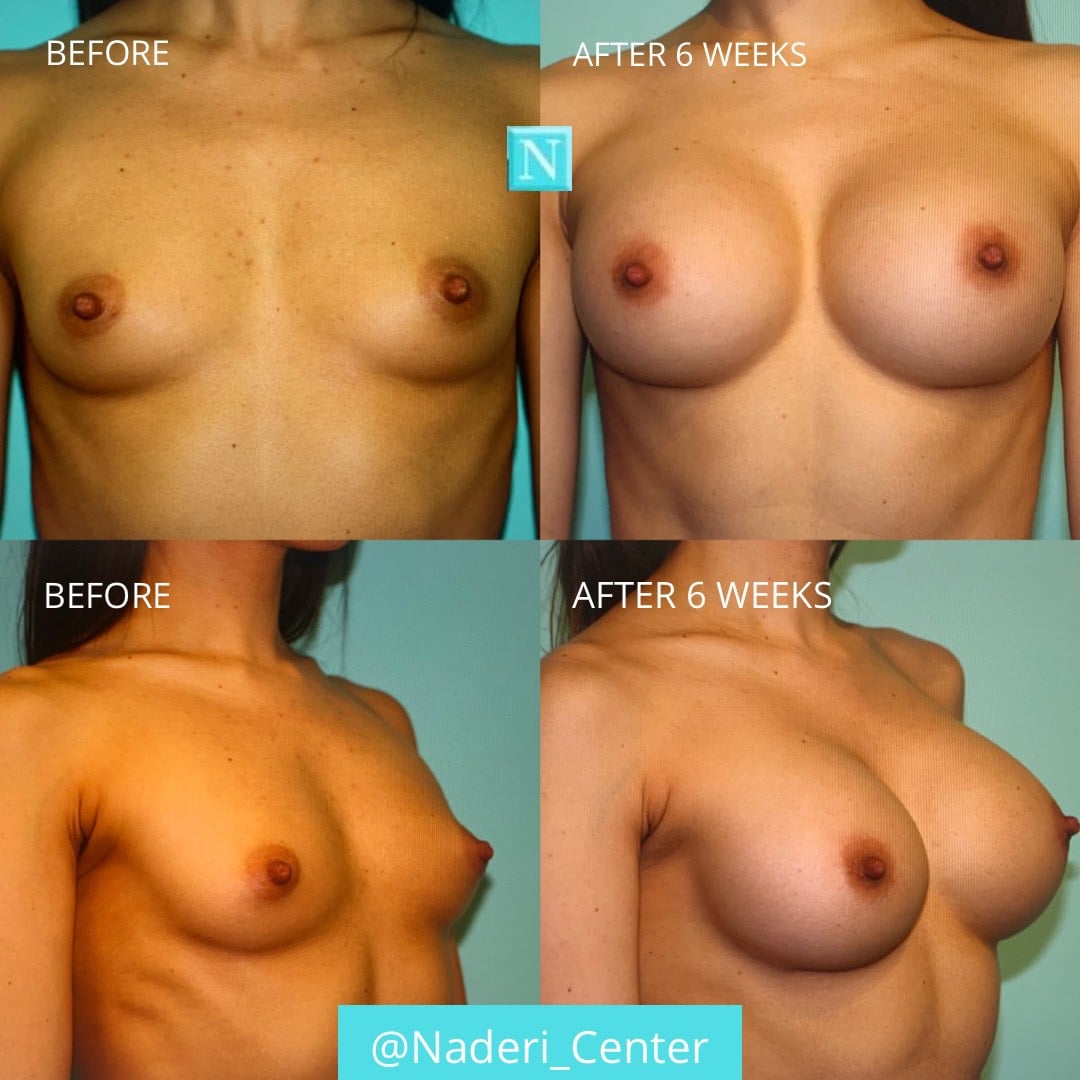
- Implant Position: Implants may appear higher in position, firm, and uneven due to swelling during the healing process. After 3-6 weeks the implants should show a more final result with significantly reduced swelling.
- Sensory Changes in Skin: You may feel reduced or heightened sensation in the nipples, incision sites, and breast tissue which is normal. You can expect return of normal sensation after a few weeks to months.
- Crackles/Sloshing Sounds: Air and fluid are left behind as a normal part of the surgery and it takes time for it to be resorbed by your body. These sounds are normal after a breast augmentation and will resolve in 5-7 days.
- Purchasing new bras: We advise waiting 8 – 12 weeks before purchasing your new size bra. During this waiting period swelling will go down and you will be able to better measure your bra size. In the interim, a t-shirt bra from Walmart or Target is a reasonable investment. Most patients like to wear their surgical bra at night only after the first post op visit.
Do Not’s During Breast Augmentation Recovery
- DO NOT apply hydrogen peroxide to incision sites. Keep postop dressings in place until follow-up.
- DO NOT soak in baths, jacuzzies or hot tubs until all incisions have fully healed.
- DO NOT take Aspirin, Ibuprofen, Naproxen, or other blood thinners until your surgeon advises you it is safe.
- DO NOT apply heating pads or ice packs to the treated areas unless otherwise instructed by your surgeon.


Emergency Situations During Breast Augmentation Recovery
WHEN TO CALL THE OFFICE (703-481-0002) OR GO TO THE HOSPITAL
- Signs of Infection: Spreading redness, worsening swelling, increased drainage or drainage of pus, worsening pain, warmth at incision site and temperature over 101°F.
- Excessive Bleeding: If the dressings are saturated with bright red blood and you are having to make very frequent dressing changes.
- Other Emergency Situations: Shortness of breath or difficulty breathing, chest pain, lightheadedness that does not quickly resolve, severe vomiting, pain, or asymmetric swelling in your legs.